Breaking Boundaries: CAR T-Cell Therapy
- Sidharth Raghavan

- Mar 18, 2021
- 6 min read
Updated: Jan 30, 2022
CAR T-cell therapy is one of the most exciting and promising innovations from the field of
biotechnology. In this article, I will unravel the history of immunotherapy, explain how CAR T-cells function, and dive into some of the latest developments in CAR T-cell therapy research.

I. A Pivotal Discovery
In the 1890s, Dr. William B. Coley, now recognized as the father of immunotherapy, made a discovery that would transform cancer research. Coley was frustrated when he was not able to save one of his first cancer patients, 17-year-old Bessie Dashiell. Surgery was the only treatment at the time and was not very effective, so he was determined to find a new solution. After scouring the files of many patients, Coley discovered that cancer patients who

acquired bacterial infections from surgery recovered better compared to those who did not acquire the infections. The immune system of the infected patients not only fought against the encroaching bacteria, but also against their cancerous tumor. This phenomenon must have been occurring for hundreds of years, however no one except Coley had the genius to connect it with the immune system. He tested his findings in a cancer patient named Zola who had very advanced, incurable tumors. A few months after Coley injected Streptococcus (a bacterium) into Zola’s tumor, Zola was able to resume his normal life and the field of immunotherapy was born.
Immunotherapy, first used by Dr. William B. Coley, consists of treatments that activate a patient’s own immune system to fight their cancer. By injecting Streptococcus in his patient’s tumor, Coley was able to activate their immune system, making it fight against the hostile bacteria. However, it turns out that the immune system did not only fight against the bacteria, but also against the tumor. Since the 1890s, Coley’s novel technique has blossomed into a promising method that could one day be applied to treat all cancers. But why is immunotherapy so promising and how does it compare to other cancer treatments?
Cancer treatments such as radiation therapy and chemotherapy are no slouch when it comes to foiling attacks from cancer cells, but they use a different approach than immunotherapy. Chemotherapy and radiation therapy use powerful drugs and light to kill cancer cells. However, they have their limitations: failing to extinguish just one cancer cell could lead to a re-growth of a deadly tumor. As the renowned author and oncologist, Siddhartha Mukherjee wrote in his book The Emperor of all Maladies, “Radiation was a powerful invisible knife - but still a knife. And a knife, no matter how deft or penetrating, could only reach so far in the battle against cancer”.
Immunotherapy, on the other hand, is much more precise because it uses weapons of a much smaller scale to attack cancer – immune cells. Lately, many scientists have recognized the potential of immunotherapy and are using it to develop new methods of fighting cancer. In the last decade, scientists unveiled a new immunotherapy weapon - CAR T-cell therapy. Scientists are excited by this treatment because its novel approach could treat patients faster than the standard treatments and be applied to a variety of cancers.
II. What is CAR T-cell Therapy?
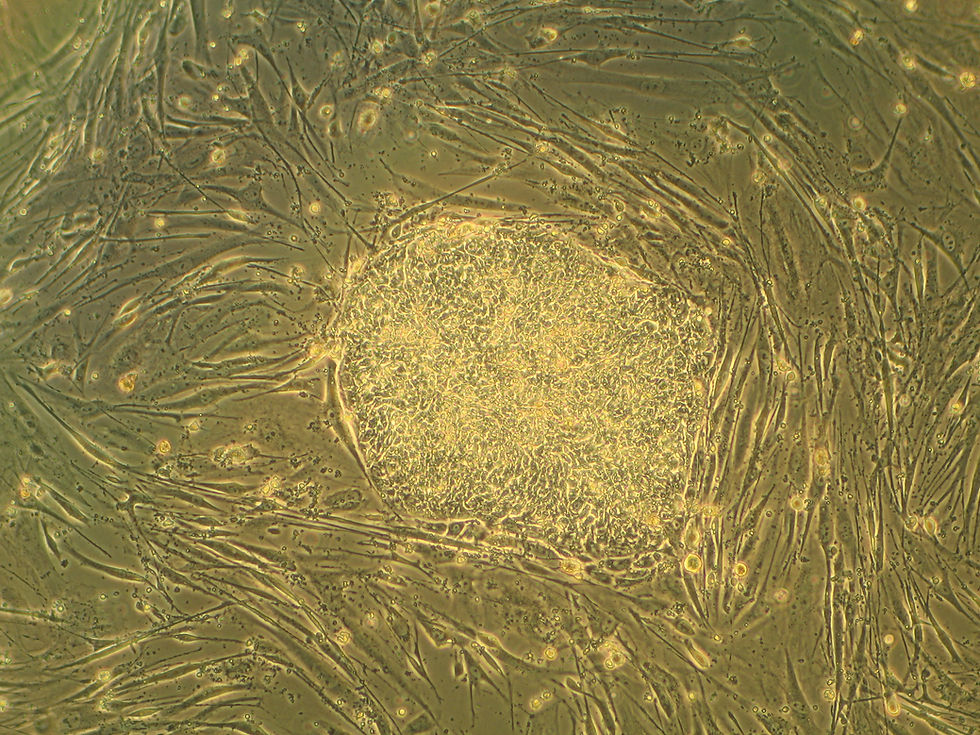
In the years following Dr. Coley’s pivotal discovery, scientists have recognized the power of T-cells - immune cells that focus on specific foreign bodies - which have the capability to search and destroy cancer cells. Unfortunately, cancer cells have many ways to deactivate the body's T cells either by producing molecules to harm them or by creating a hostile environment around them. Zelig Eshhar, an immunologist at the Weizmann Institute of Science in Rehovot, Israel, was the first to engineer CAR T-cells in an attempt to solve this

problem. Antibodies are proteins that can recognize and stick to certain proteins. By attaching an antibody to the receptor of a T-cell, Eshhar created ‘first generation’ CAR T-cells. CAR (chimeric antigen receptor) proteins are unique because they are programmed via an antibody to recognize a specific cancer cell, precisely the cancer cell’s antigen. CAR T-cells are built by extracting T-cells from the patient’s body and injecting them with the DNA code for a specific CAR protein. Now, when introduced in a cancer patient, the CAR T-cells will be able to produce enough warriors to recognize and fight off the tumor.
Cancer is an elaborate disease; therefore, each CAR T-cell treatment will differ depending on the patient as to not induce a large immune reaction. Thus, at the moment, CAR T-cell therapy is only clinically used for some kinds of lymphomas and leukemias. Now, scientists are attempting to expand its use to other types of cancers.
One of the first CAR T-cell therapies to be approved was for acute lymphoblastic leukemia (ALL). Out of a study with 30 children, 27 of them (90%) demonstrated a complete response rate in treating the ALL with CAR T-cells. This is great evidence showing that CAR T-cell therapy is effective at treating some cancers however, there is still more work to be done. CAR T-cell therapy works, but it can be further developed to make it more safe, effective, and versatile.
III. Breaking Boundaries
CAR T-cells have proved to be a worthy fighter against lymphomas and leukemias, both of which are liquid tumors, occurring in the blood or bone marrow. However, CAR T-cells have a hard time fighting against solid tumors – cancers that affect organs. These tumors are challenging for regular CAR T-cells to destroy because they consist of thick layers of cells, produce chemicals to suppress the immune system, and contain cells with different types of antigens. In 2018, scientists at Memorial Sloan Kettering Cancer Center made a crucial leap. They combined CAR T-cells with checkpoint inhibitors, the ‘break mechanism’ on T-cells, allowing them to fight against cancer more effectively. The protein PD-1 is responsible for inactivating T-cells; the new CAR T-cells release antibodies that attach to PD-1, not only reversing the suppression of the T-cells, but also recruiting support from the bodies’ T-cells to fight the cancer. Now, the immune system has a better force to battle the solid cancer.

These new weapons, called armored CAR T-cells, hold immense promise. When tested in mouse models of solid tumors, researchers found that the mice lived longer and that armored CAR T-cells were more effective than normal ones. In 2018, Dr. Reiner Brentjens, the pioneer of this novel method, commented “This proves – at least in a mouse model – that we can now have our cake and eat it too”. Recently, a clinical trial by Innovative Cellular Therapeutics involving armored CAR T-cells showed that they had a 92% response rate and a 53% complete response rate on cancer patients.
It is clear that CAR T-cell therapy works on cancer patients with certain types of tumors; however, CAR T-cell therapy is expensive, and it can take weeks to create the therapy. In making CAR T-cells scalable and more accessible, one method that appears elusive is designing CAR T-cells that target common tumors. Doctors could make a CAR T-cell ‘cocktail’ for their patients. However, there are numerous problems with this approach, the first and foremost being the risk of a large and potentially life-threatening immune reaction. The human body’s immune system rejects foreign bodies, so it could also reject the scalable CAR T-cells. Last year, Dr. Maksim Mamonkin and his fellow scientists at the Baylor College of Medicine made a groundbreaking discovery by developing scalable CAR-T cells that could one day make the therapy cheaper and more accessible to patients who need it. In addition to expressing the CAR protein, his novel CAR T-cells expressed an alloimmune defense receptor protein (ADR). T-cells and natural killer (NK) cells are responsible for the body’s immune reaction and destroy foreign bodies. The ADR is able to halt some of the processes in the T-cells and NK cells, allowing the new CAR/ADR T-cells to flourish in the body. Ultimately, Mamonkin developed the backbone for scalable CAR T-cells that escapes the worry of a lethal immune response.
IV. Conclusion
From Coley’s discovery in the 1890s to Mamonkim’s creation in 2020, the field of immunotherapy has progressed far. In the next decade, scientists will need to work on making CAR T-cell therapy safer, more effective, and cheaper. Severe immunological reactions can arise due to CAR T-cell therapy, and those need to be fixed either by altering the CAR T-cell therapy itself, or by finding drugs to hamper the reactions. Cancer is a disease that presents itself differently depending on the patient. My hope is that with the latest developments in CAR T-cell therapy, a method is derived to take any patient's cancer and forge an effective CAR T-cell therapy to cure it.


Way to go Sid!!